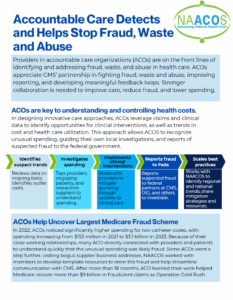
Value-Based Care Detects and Helps Stop Fraud, Waste and Abuse
Providers in accountable care organizations (ACOs) are on the front lines of
identifying and addressing fraud, waste, and abuse in health care. ACOs appreciate CMS’ partnership in fighting fraud, waste and abuse, improving reporting, and developing meaningful feedback loops. Stronger collaboration is needed to improve care, reduce fraud, and lower spending.
Download our fact sheet to learn more about the role ACOs play in detecting and stopping fraud, waste, and abuse, as well as actions the Centers for Medicare and Medicaid Services can take to better partner with ACOs in the fight against bad actors.