Survey Shows ACOs’ Concerns About the Effect of COVID-19
Overview
In addition to the significant toll the COVID-19 pandemic is having on our healthcare and economic systems, new survey results show the global pandemic could derail a decade-long effort to shift payment for healthcare services from a focus on volume to one on value. Value-based payment models, such as accountable care organizations (ACOs), incentivize physicians, hospitals, and all healthcare providers to work in a more coordinated manner, focusing on delivering high-quality care while avoiding unnecessary utilization and costs. An increasing number of providers have embraced the ACO model and its focus on accountability for cost and quality, but new survey results demonstrate that normal accountability is not appropriate in the face of a global pandemic.
In early April, the National Association of ACOs (NAACOS) emailed all Medicare Shared Savings Program (MSSP) and Next Generation ACO Model participants, including NAACOS members and nonmembers, with a request to complete an online survey focused on the effects of COVID-19 on ACOs. There were 304 responses from 226 ACOs across the country. The results of that survey send a clear and strong message that ACOs are very concerned about the effects of COVID-19 on their ACO. As shown in more detail below, those worries are illustrated by almost 60 percent of respondents in risk-based models reporting they are likely to quit the ACO program to avoid financial losses stemming from the pandemic, and 77 percent of ACOs reporting they are “very concerned” about the impact of COVID-19 on their ACO’s 2020 performance.
What are ACOs doing to help fight the pandemic?
Survey Findings
A vast majority of ACOs are very concerned about the effect of COVID-19 on their ACO
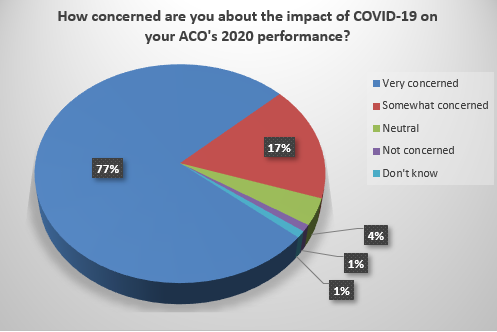
When asked how concerned ACOs are about the impact of COVID-19 on their ACO’s 2020 performance, 77 percent report being “very concerned” and 17 percent report being “somewhat concerned.” The remaining 6 percent of responses were split between being not concerned, neutral, or don’t know.
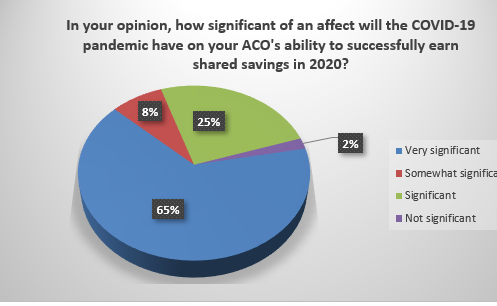
Further, 90 percent of ACOs report that the COVID-19 pandemic will have a significant or very significant effect on their ACO’s ability to earn shared savings.
While the concept of foregoing shared savings may seem like a small price to pay in an economy teetering on the brink of significant recession, shared savings payments for ACOs are often the only funding they have to keep the ACO functioning. Medicare does not pay ACOs a per-member, per-month or per-year payment, nor does it provide additional support to fund ACO operating costs that go towards additional clinical resources, data analytics, care coordinators, health IT, compliance, or administration.
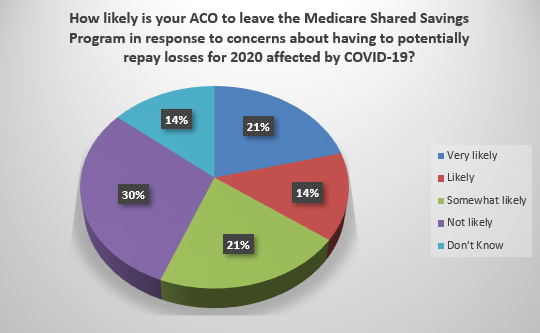
A large portion of risk-based ACOs are likely to quit over concerns about COVID-19
In response to an emphasis in recent years for ACOs to assume increasing levels of financial risk, currently more than 40 percent of Medicare ACOs are in risk-based models. The MSSP has a May 31 deadline for risk-based ACOs to give notice of quitting to avoid losses, as well as potential savings opportunities, for this year. The survey found that 56 percent of risk-based MSSP ACOs report they are likely to leave the MSSP in response to concerns about having to potentially repay losses in 2020 because of COVID-19.
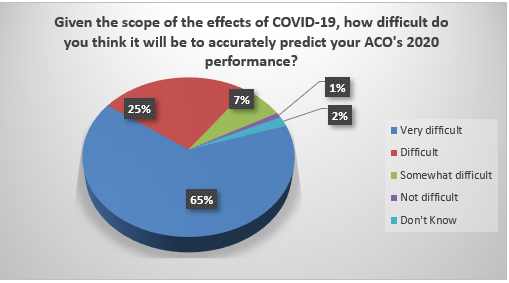
Uncertainty and difficulty predicting performance are notable concerns
A likely driver for ACOs to quit the program is the uncertainty about costs, quality, and utilization for 2020. COVID-19 has upended normal utilization and care patterns, disrupting ACOs’ ability to employ successful population-health strategies and causing tremendous uncertainty about costs. There is also notable uncertainty on how the pandemic will affect other aspects of the ACO program, such as changes to acuity or risk scores, diminished opportunities to meet quality requirements related to preventive care, and which patients the ACO will be accountable for this year. This uncertainty was strongly noted by survey respondents in comments, and 65 percent reported that the scope of the effects of COVID-19 will make it very difficult for them to accurately predict their ACO’s 2020 performance.
CMS’s “Pathways to Success” regulations were finalized in late 2018 and overhauled the MSSP in many ways. The agency made certain changes to provide more stability and predictability for ACOs, which NAACOS supported. Without stability, ACOs are reluctant to assume financial risk and do not know how to properly plan for the short and long term. These survey results indicate that predictability is impossible for 2020. With little hope for predictability, financial accountability becomes an even riskier proposition.
ACOs anticipate notable increases in 2020 Medicare spending from COVID-19
Increased uncertainty about performance is tied in large part to what the net effect of COVID-19 will be on each ACO’s performance year expenditures. There is considerable variability across the country. Certain areas are designated as COVID-19 hotspots, while others are seeing very low numbers and bracing for possible surges in infection rates and deaths in the coming weeks and months. At the same time, there is a significant decline in elective procedures and routine preventive care. When asked to provide their best estimate of the net effect of COVID-19 on their ACO’s 2020 expenditures, respondents gave a range of answers with a majority, 53 percent, predicting increased spending and almost 40 percent of respondents selecting “don’t know.”
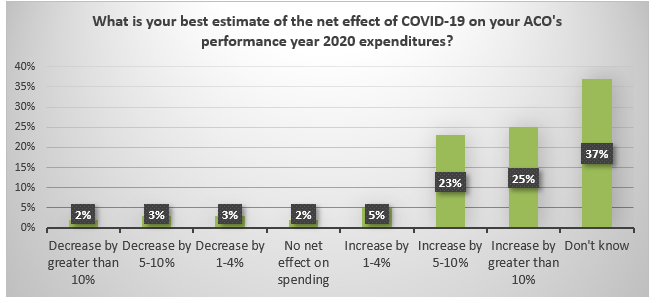
To put these numbers in context, for 2018 (the most recent year for which ACO results are available), MSSP ACOs that earned shared savings had expenditures that were, on average, 4.8 percent lower than benchmarks. ACOs owing shared losses had expenditures 2.1 percent higher than benchmarks on average.
The Importance of Keeping ACOs Engaged in Value
The ACO model has gained traction in recent years, showing improved quality and savings to Medicare, as noted in the box to the right. Medicare ACO programs have grown in size in recent years and 12 million beneficiaries are assigned to ACOs, representing roughly 20 percent of Medicare. There are also more than 500,000 clinicians in ACOs and roughly 1,500 hospitals participating. Along with that growth has come an increasing number of ACOs that are liable for spending that exceeds preset targets, or benchmarks, which are based on historical spending data from previous years. Those targets will not be meaningfully updated to reflect the expected spike in spending many experts predict will happen this year, resulting in ACOs paying Medicare for the costs of a global pandemic. It’s important to emphasize that Medicare ACO models are voluntary programs, which providers can quit and return to a traditional fee-for-service environment. When this happens, care coordination programs are redirected away from Medicare patients, less attention and effort is put into analytics used to track and treat patients, quality programs are dissolved, and unnecessary utilization is no longer monitored or addressed. Policymakers should do everything they can to avoid these negative effects on patient care, outcomes, and the Medicare Trust Fund.
The Importance of Keeping ACOs Engaged in Value
The ACO model has gained traction in recent years, showing improved quality and savings to Medicare, as noted in the box to the right. Medicare ACO programs have grown in size in recent years and 12 million beneficiaries are assigned to ACOs, representing roughly 20 percent of Medicare. There are also more than 500,000 clinicians in ACOs and roughly 1,500 hospitals participating. Along with that growth has come an increasing number of ACOs that are liable for spending that exceeds preset targets, or benchmarks, which are based on historical spending data from previous years. Those targets will not be meaningfully updated to reflect the expected spike in spending many experts predict will happen this year, resulting in ACOs paying Medicare for the costs of a global pandemic. It’s important to emphasize that Medicare ACO models are voluntary programs, which providers can quit and return to a traditional fee-for-service environment. When this happens, care coordination programs are redirected away from Medicare patients, less attention and effort is put into analytics used to track and treat patients, quality programs are dissolved, and unnecessary utilization is no longer monitored or addressed. Policymakers should do everything they can to avoid these negative effects on patient care, outcomes, and the Medicare Trust Fund.
Evidence of ACO Savings and Quality
Conclusion
This brief survey provides a snapshot of ACOs’ concerns about COVID-19. It does not capture the myriad of positive stories about how ACOs are contributing to the fight against this global pandemic. ACO providers are on the front lines treating patients and supporting their communities. Additionally, ACOs are uniquely positioned to support the response to COVID and have diverted typical ACO resources such as clinicians, analytics, health IT, administration, and funding to support this fight.
The survey results detailed above paint a potentially grim picture for ACOs and the move to value. Advancing value-based care has been a priority of Congress and the administration. If the Department of Health and Human Services’ goal remains moving all Medicare payments into alternative payment models by 2025, then it is imperative that the government appropriately adapt models to withstand the highly unusual circumstances brought on by COVID-19. Specifically, NAACOS and other leading healthcare organizations are calling on Congress and the administration to cancel all losses for ACOs for Performance Year 2020. More ACOs have assumed downside risk in recent years, which has been a priority for the administration. Simply put, ACOs’ acceptance of financial risk did not account for a global pandemic. ACO providers are risking their lives treating COVID-19 patients, they should not also be required to risk their businesses, many of which are not equipped to potentially pay millions to the government for increased costs from COVID-19. As our nation and healthcare system recover from this pandemic, we will need ACOs more than ever. They should be protected now to enable them to continue the tremendous work they are doing to improve quality and patient care while bending the cost curve.
