FOR IMMEDIATE RELEASE: October 23, 2025
Contact: Tamara Moore, [email protected], (202) 908-6899
Medicare Skin Substitute Spending on Track to Hit $15.4 Billion in 2025
Analysis by National Association of ACOs and Institute for Accountable Care projects 55% increase in spending
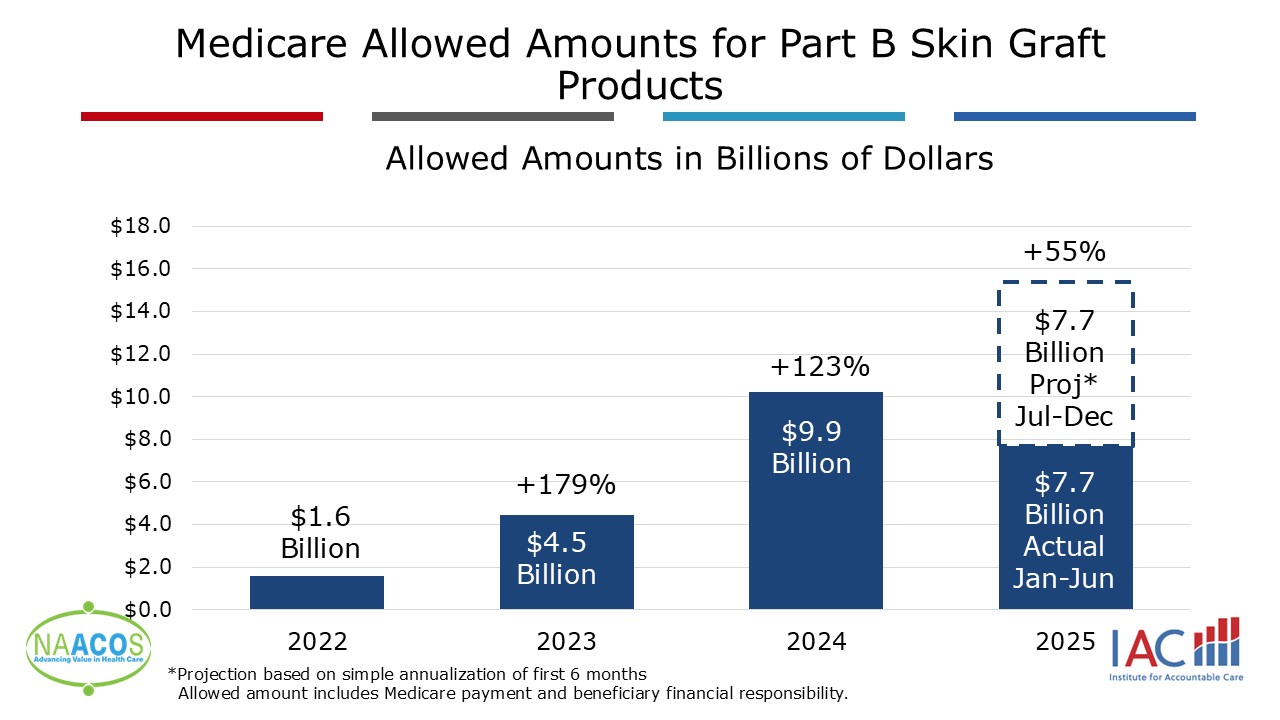
WASHINGTON (October 23, 2025) – A new analysis of Medicare data by the National Association of ACOs and the Institute for Accountable Care shows that spending on skin substitute products reached $7.7 billion through July 2025 and is projected to reach $15.4 billion by the end of 2025, a 55% increase over 2024 spending. The accelerated spending comes as many accountable care organizations (ACOs) seek action by the Centers for Medicare & Medicaid Services (CMS) to address payment flaws and ensure ACOs are held harmless for fraud, waste, and abuse that occur beyond their control.
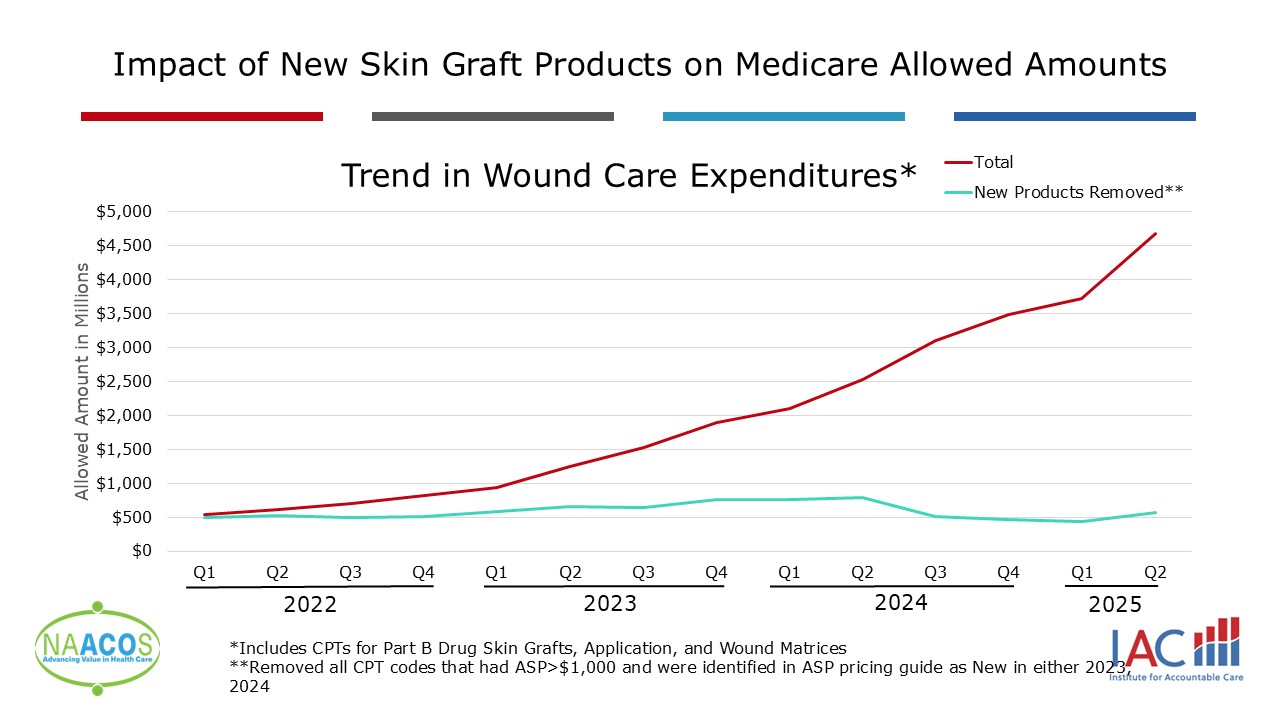
Since 2023, 102 new skin substitute products have entered the market, including more than 50 in 2025 alone. The average sales price (ASP) varies, but 69 products cost more than $1,000 per square centimeter, and some cost up to almost $6,000 per square centimeter. Without the new products, spending from 2022 through July 2025 would have been reduced by more than 70%.
“The deliberate misuse of skin substitutes is endangering America’s seniors and pricing schemes are undermining the integrity and the long-term sustainability of Medicare,” said Emily Brower, president and chief executive officer of the National Association of ACOs. “If we are truly committed to combating fraud, waste, and abuse, we must put an end to this exploitation by bad actors.”
In July, CMS proposed a rule to shift payment of skin substitutes for Medicare beneficiaries to be billed as supplies used for wound care procedures on an incident-to basis, rather than paying based on skin substitute products’ specific ASP. Additionally, CMS would establish an initial payment rate of $125.38 per square centimeter. If finalized and enacted in January 2026, this proposed policy has the power to save the government $9.4 billion. Several legislative efforts related to skin substitutes have also been introduced to address the exorbitant spending but would not rein in spending as much as the CMS proposed rule.
Additionally, the Department of Health and Human Services’ Office of the Inspector General recently published a report highlighting concern about skin substitute payment trends. Beyond skyrocketing spending, the analysis identified a massive gap in patient use and utilization and spending between traditional Medicare and Medicare Advantage—both of which cover similar patient populations—highlighting the loopholes that have led to inappropriate use.
“We appreciate attention to skin substitute payment flaws, but every day that passes, Medicare loses millions of dollars to wasteful, unnecessary spending that does not improve the health of seniors,” said Aisha Pittman, senior vice president of government affairs for National Association of ACOs. “Accountable care organizations are Medicare’s strongest defense against fraud, waste, and abuse—delivering high-quality care in patients’ best interests. But they cannot be held responsible for tens of billions of dollars in inappropriate spending that they have no control over.”
NAACOS members have reported an increase in utilization since the CMS proposed rule was released in July, as well as noting that skin substitute providers have been holding claims before submitting to Medicare for reimbursement. This delays the timeline of notification to ACOs, limiting opportunities to intervene.
The misuse and spending has hit small ACOs and those that treat the most complex patients the hardest. Small providers are more impacted by outlying high-cost cases. Additionally, complex patient populations tend to have conditions that require wound care, making these seniors more at risk of predatory practices.
To strengthen and retain competition in health care through sustainable accountable care models, NAACOS and others have asked CMS to refine program policies to ensure ACOs are held harmless for fraud, waste, and abuse that occur beyond their control.
###
The National Association of Accountable Care Organizations (NAACOS) is a member-led, member-governed nonprofit of nearly 500 ACOs and value-based care entities in Medicare, Medicaid, and commercial insurance working on behalf of physicians, health systems, and other providers across the nation. These value-based care providers seek to improve the quality of care while reducing costs. NAACOS represents more than 9 million beneficiary lives through Medicare’s population health-focused payment and delivery models.