April 22, 2016
Mr. Andrew Slavitt Acting Administrator
Centers for Medicare & Medicaid Services
U.S. Department of Health and Human Services
Hubert H. Humphrey Building
200 Independence Avenue, S.W.
Washington, DC 20201
Subject: Improving the Adoption and Cost Savings of the Comprehensive Primary Care Plus (CPC+) Program by Allowing ACO Participation
Dear Administrator Slavitt:
The National Association of ACOs (NAACOS) supports CMS’ efforts to enhance primary care through the CPC+ program and strongly urges CMS to allow ACO participation. ACOs inherently value comprehensive primary care and enthusiastically support expanded access to comprehensive primary care through the CPC+. Many ACOs have successfully combined per beneficiary per month payments for comprehensive primary care and shared savings based on total cost of care in the commercial market, and we believe that CPC+ presents an opportunity to bring that success to Medicare beneficiaries.
NAACOS is the largest association of Medicare ACOs, representing over 3 million beneficiary lives through 180 Medicare Shared Savings Program (MSSP) ACOs, Next Generation, Pioneer and commercial ACOs.
NAACOS is an ACO member-led and member-owned non-profit organization that works on behalf of ACOs across the nation to improve the quality of Medicare delivery, population health and outcomes, and health care cost efficiency. Our members, more than many other healthcare organizations, want to see an effective, coordinated patient-centric care process. Our recommendations in this letter reflect our expectation and desire to see the MSSP achieve the long-term sustainability necessary to enhance care coordination for Medicare beneficiaries, reduce healthcare costs, and improve quality in the Medicare program.
Implications of Current CPC+ Policies on ACOs
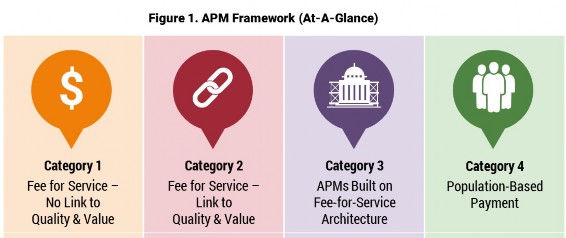
Although we support the concept of this new initiative, we are very concerned that the CPC+ program requires physicians to choose between MSSP participation and being supported directly for providing comprehensive primary care through CPC+. By putting primary care practices in this either/or position, CMS will slow the adoption of accountability for total cost of care, the greatest opportunity to bend the cost curve. CMS has repeatedly indicated its desire to move physicians along the continuum from fee for service to value-based care. CPC+ is an ideal option for primary care providers firmly in fee for service as it helps move them on the continuum by linking fee for service to quality and value, as depicted by the Health Care Payment and Learning Action Network framework below. However, by excluding ACOs from CPC+, there will be a negative unintended consequence of incentivizing ACO primary care providers to exit the MSSP in order participate in CPC+, essentially shifting those in Category 3 back to Category 2. Many of those ACO providers are still gaining experience and should be supported, rather than penalized, for their early efforts to move along the continuum.
Health Care Payment and Learning Action Network, Alternative Payment Model Framework
With only a paltry maximum of $24 per beneficiary per year at risk for total cost of care (based on the $2.00 per month performance-based utilization payment in CPC+ Track 2), a primary care physician in CPC+ is incentivized to focus on care delivery not controlling the total cost of care. Economically, physicians could generate similar additional revenue from participating in CPC+ as they would in succeeding in MSSP, but CPC+ does not require they assume any meaningful risk for success in achieving cost savings. Additionally, CPC+ does not even necessitate the investment risk present in Track 1 MSSP since CPC+ provides an ongoing payment stream to fund the practice investments.
Of the 86 MSSP ACOs that earned shared savings in 2014, per beneficiary per month savings ranged from
$6.54 to $79.80, with a mean of $26.05. Unfortunately, only a quarter of 2014 ACOs earned shared savings, illustrating the challenges ACOs face achieving savings. Given the option of pursuing uncertain shared savings through MSSP or receiving comparable guaranteed payments through CPC+ as well as additional payments under this program, we are deeply concerned many will choose the latter. Based on the uncertainty of achieving shared savings through MSSP and having to forego opportunities such as CPC+, CMS is asking ACOs to take on risk without any additional benefits. Excluding ACOs from CPC+ could significantly undermine the MSSP, impacting existing ACOs that may have primary care practices leave the ACO to pursue CPC+ and deterring primary care practices from joining of forming their own ACO. This is a detrimental outcome for ACOs and Medicare, which would lose future shared savings and quality improvements by ACOs.
Furthermore, the timing of CPC+ selection combined with the timing of the MSSP application cycle has the potential to paralyze the decision making process for primary care providers. It requires a significant investment to apply for the MSSP, resources that may be put aside in hopes of being in one of the 20 regions selected for CPC+. If primary care practices leave an ACO or do not apply for the MSSP because they are holding out for CPC+ and are not in a chosen CPC+ region, they will be left in a fee for service only world for yet another year.
Recommendations
We believe the CPC+ program would gain substantially more adoption, have a greater impact on lowering total cost of care, and accelerate the Administration’s policy of moving to value-based care if primacy care practices in existing and new Medicare ACOs were allowed to participate in CPC+. We urge CMS to reverse its initial decision to exclude Medicare ACOs from participating in CPC+ and allow ACOs to be eligible to participate. We understand CMS considers both of these to be shared savings programs, which was the impetus for excluding ACOs. However, CMS can easily avoid an overlap in shared savings by allowing ACOs to participate in CPC+ but replacing the $2.50 or $4.00 monthly performance-based incentive payment with MSSP participation and accountability for total cost of care. With this revision, ACOs would only be eligible to earn shared savings through the MSSP but would be able to benefit from the CPC+ monthly care management fees. Because comprehensive primary care, when executed effectively, is designed to lower downstream costs, we feel it would be appropriate to include CPC+ care management fees in ACO total costs and shared savings calculations.
This proposed solution would also provide CMS an additional comparison group for the both CPC+ and the MSSP and would accelerate progress towards the goals the Secretary set to move 50% of payments to value- based payment models by 2018. We believe that, as introduced, CPC+ will slow the move from fee for services to value-based care, but we are heartened that a simple solution exists to both make the model a better experiment for CMMI and to turn the program into an accelerator in the move to value-based care.
Conclusion
We share CMS’s commitment to achieving a long-term successful ACO model for Medicare, which will enhance beneficiary care, improve quality and generate savings to the Medicare Trust Funds, and we strongly urge CMS to include ACOs in CPC+ and similar opportunities. By including ACOs, many of which are still on the preliminary learning curve, CMS would support them rather than undermine them by excluding them from these opportunities which could help them achieve success. We appreciate CMS’s consideration of our concerns and recommendations and gladly make ourselves available to assist in any way as CMS moves towards value-based healthcare.
Sincerely,

Clif Gaus President and CEO
Cc: Patrick Conway, Deputy Administrator for Innovation & Quality, CMS Chief Medical Officer
