News Release
January 10, 2020
Contact:
David Pittman
NAACOS Health Policy and Communications Advisor
202-640-2689
[email protected]
CMS Announces 2020 Medicare ACO Class and Next Generation ACO Savings
NAACOS calls on Congress to examine Medicare’s 2018 changes to key ACO program
WASHINGTON — Overall participation in the Medicare Shared Savings Program (MSSP), the country’s dominant value-based payment program, remained flat, following landmark changes the Centers for Medicare & Medicaid Services (CMS) enacted in 2018. Today’s data show 517 ACOs are participating in the program in 2020, down from a high of 561 two years ago and 518 last year. Importantly, 11.2 million beneficiaries – more patients than ever – are being care for by ACOs, and nearly 200 ACOs are taking on down-side risk.
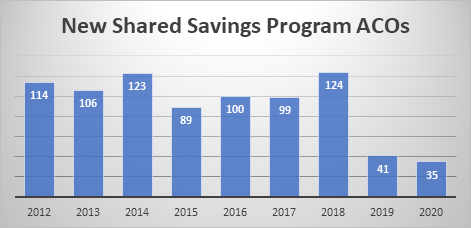
However, this year just 35 Shared Savings Program ACOs will enter into their first contract with CMS. Between 2012 and 2018, the program averaged 107 new ACOs annually. Last year was the first time the program saw a drop in overall participation when just 41 new ACOs joined. In the fall of 2018, CMS overhauled the Shared Savings Program to force ACOs to take on risk sooner while at the same time reducing the portion of savings ACOs can keep. NAACOS and other health provider associations warned the changes could harm Medicare’s move to value-based payment by hindering participation in a voluntary program.
In a Health Affairs blog last fall, NAACOS urged policymakers to pay close attention to participation numbers released today as CMS’s efforts to move ACOs into risk would be undermined if fewer ACOs participate in or enter the program.
“ACOs have had the greatest success of any of Medicare’s payment reform efforts,” said Clif Gaus, Sc.D., president and CEO of the National Association of Accountable Care Organizations (NAACOS). “If interest in ACOs dwindles, then doctors and hospitals will fall back into a fragmented, fee-for-service system, and any momentum to transform our health system will be lost.”
“NAACOS feared that changes CMS made under Pathways would throw off the careful balance of risk and reward for too many ACOs. Sadly, those fears may be coming true,” Gaus said. “To date, there have been few attractive alternative payment models besides ACOs, so harming participation in the Medicare Shared Savings Program hurts Medicare’s priority of changing how it pays for care. Congress should take a closer look at this program to ensure more damage isn’t done.”
Data increasingly show ACOs are reducing Medicare spending. ACOs collectively saved Medicare $1.7 billion in 2018 alone, and $739 million after accounting for shared savings bonuses and collecting shared loss payments. Last year, the Medicare Payment Advisory Commission reported MSSP reduced spending between 1 and 2 percent from 2013 to 2016, which translates into tens of billions of dollars when compounded annually. An independent analysis commissioned by NAACOS and conducted by a health economics and policy consulting firm showed $3.53 billion in overall savings and more than $755 million in net savings, after paying shared savings to ACOs.
2018 NEXT GENERATION ACO RESULTS
Medicare’s most advanced, greatest risk-taking ACOs – the Next Generation ACO Model (Next Gen) – collectively saved Medicare $406 million last year, according to 2018 performance data made public. Importantly, these ACOs also hit an average quality score of 93 percent, improving care for 1.4 million seniors. After accounting for shared savings paid to ACOs for holding down costs and hitting quality targets as well as shared losses paid back to the government, the Next Gen program netted $185 million to Medicare last year alone. These figures are impressive especially considering this program only had 50 Next Gen ACOs participating last year.
The Next Generation ACO Model is due to sunset at the end of this year. NAACOS and others have called on CMS to make the program a permanent fixture, either as a stand-alone program or an option within the MSSP. ACOs could use Next Gen as an additional option when contemplating participation in Direct Contracting and other ACO models in 2021 and beyond.
“The Next Gen program has been very successful, focusing on the CMS Innovation Center’s goals of lowering spending and improving quality,” Gaus said. “CMS should recognize the contributions of these ACOs and this program and continue it as an alternative payment model for years to come.”
The Next Gen program netted at least $165 million to Medicare in 2017, after accounting for shared savings paid to ACOs for holding down costs and hitting quality targets as well as shared losses paid back to the government. That year, 44 Next Gen ACOs participated in the program, serving 1.2 million Medicare patients.
An independent evaluation of the program was also released today but the results are not as positive as the 2018 CMS results. This evaluation follows one on the first year of the program which showed that 18 Next Gen ACOs saved Medicare $62 million in 2016, after accounting for incentive payments earned for hitting spending and quality targets. Every other data point on the Next Gen program has been positive to date, so we look forward to further understanding today’s formal evaluation. Importantly, the comparison group used included MSSP patients, rather than non-ACO patients, which could limit results.
